Case Review
History
• 68-year-old female
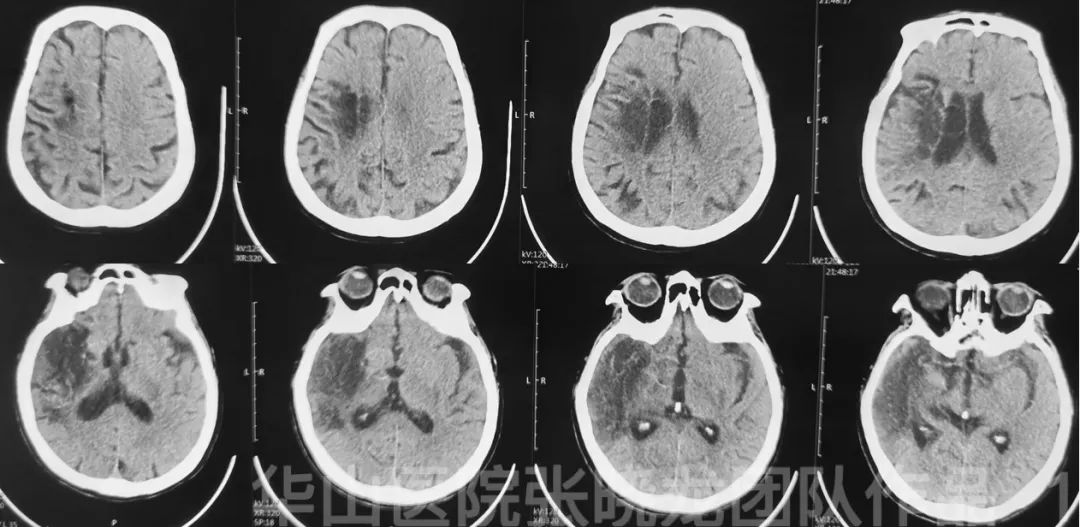
Figure 1. CT taken on 2021/05/10 shows right frontal and temporal lobe chronic infarctions. No evidence of right MCA calcification.
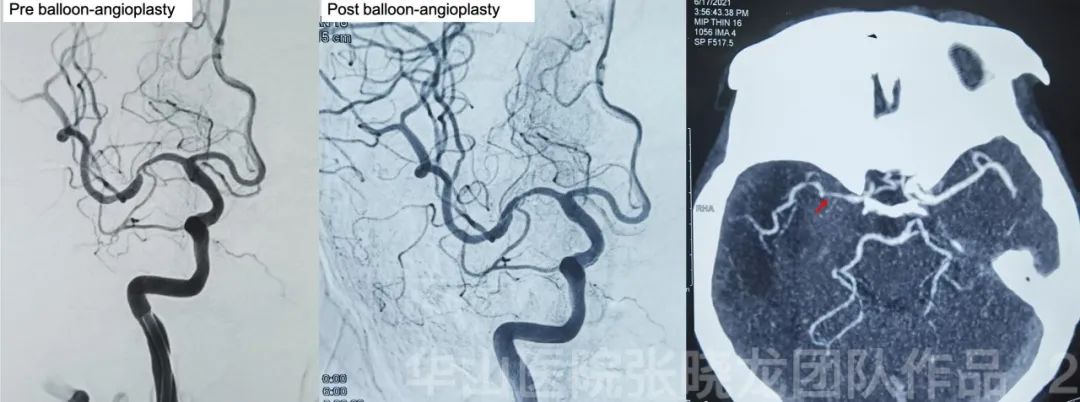
Figure 2. The right MCA severe stenosis was dilated by balloon.But one-month follow up CTA shows severe re-stenosis of the right MCA.
Figure 3 GIF. Multiple arteriosclerotic stenosis of bilateral PCAs. Pial collateral compensation from right PCA are noted.
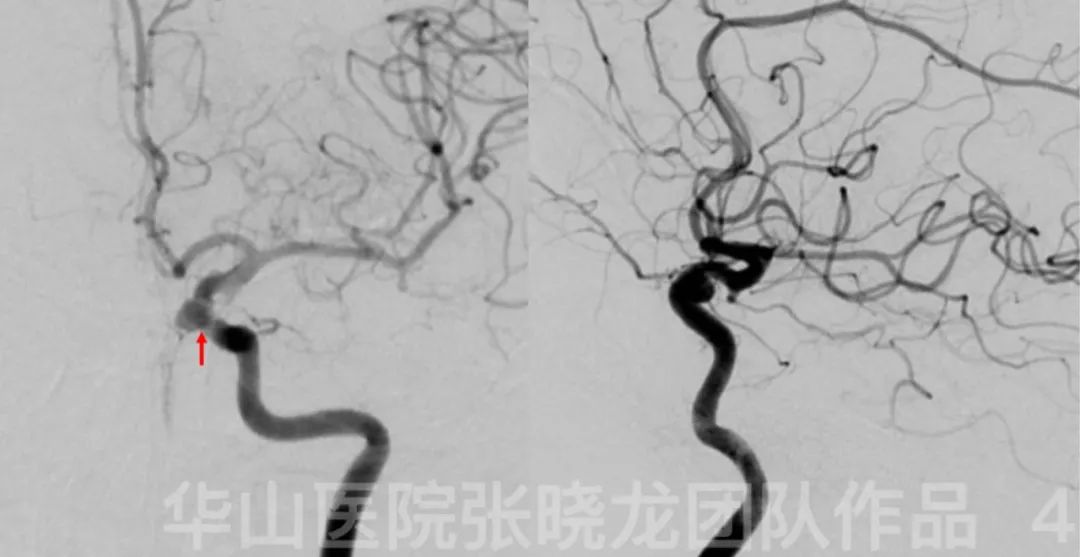
Figure 4. A small carotid-ophthalmic aneurysm was found incidentally.
1
Strategy
• The symptoms were caused by severe right MCA stenosis. Although balloon angioplasty was performed, CTA revealed re-stenosis occurred. Furthermore, the symptoms persisted and worsened, therefore stenting has become necessary.
2
Operation
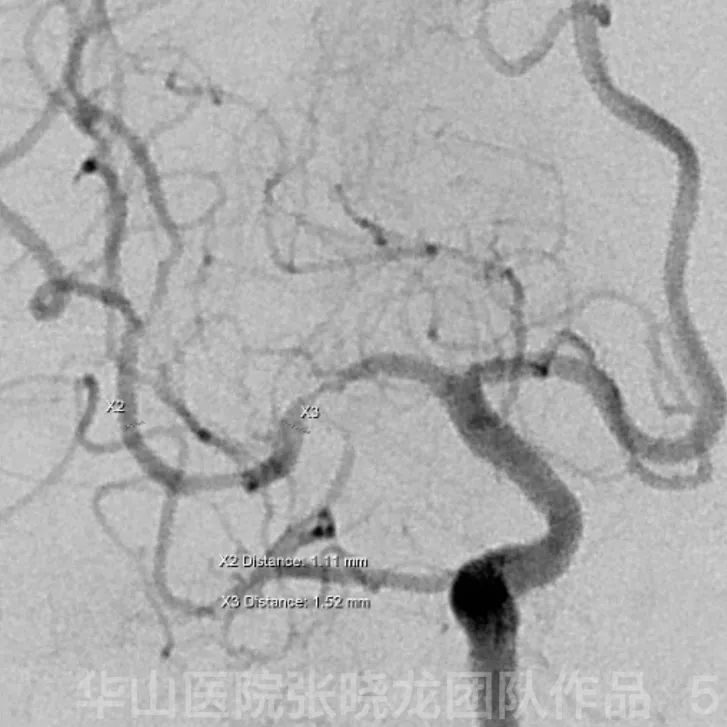
Figure 5. A proper working projection was selected to avoid any skeletal artifact and reveal the right MCA clearly.
Video 1. General heparinization. Gateway 1.5*15mm balloon was navigated to the stenotic segment guided by Floppy-300 microwire. The vessels shifted when the microcatheter crossed the MCA.
Figure 6 GIF. The stenosis was dilated by balloon under 7 ATM for 60s. Nimodipine 1ml was administrated after balloon angioplasty.
Video 2. Wingspan 2.5*15mm was deployed covering the stenosis.
Video 3. The delivery system became entangled with the distal end of the stent requiring repeated adjustment of the microwire.
Figure 7 GIF. Angiography shows the revascularization of the stenosis.
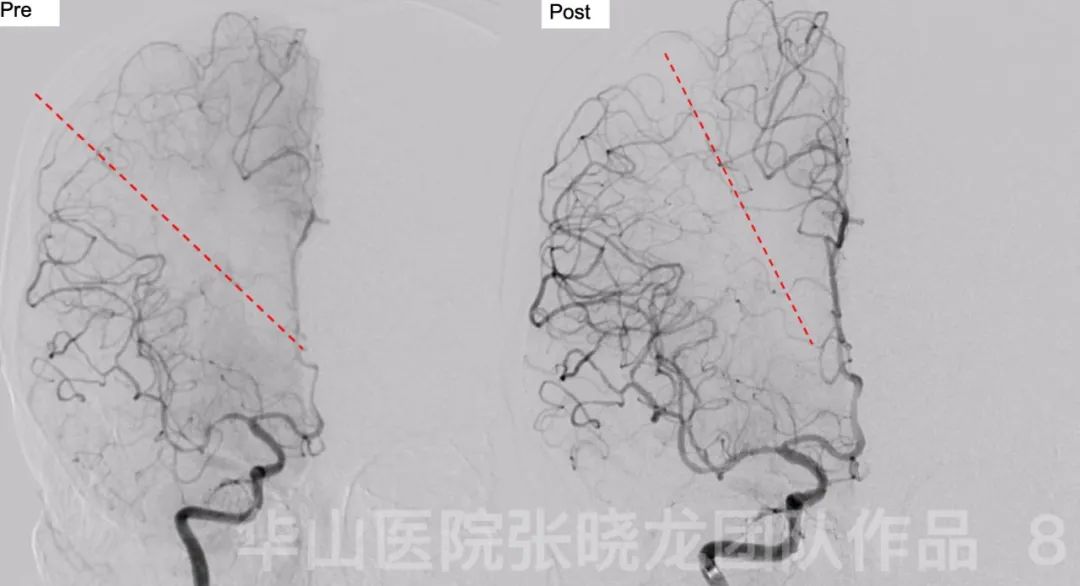
Figure 8. The watershed line migrated after the operation indicating increased flow in the right MCA territory.
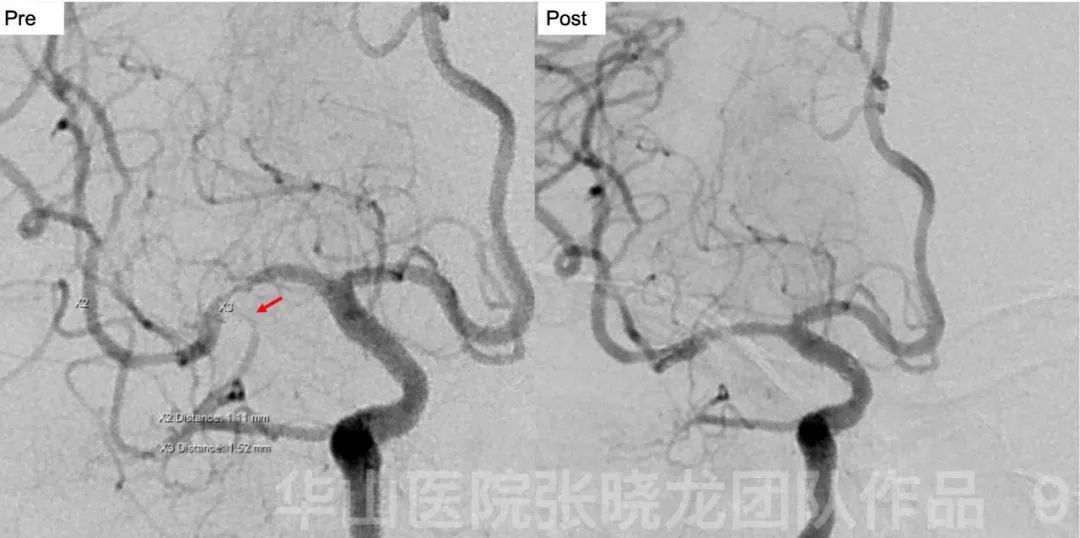
Figure 9. However, compared to the span-angioplasty angiography, the inferior trunk occlusion is noted in the post-angioplasty angiography, which could be due to plaque dislogement after stenting.
Figure 10 GIF. Pial collateral compensation to the region of occluded inferior MCA branch is noted.
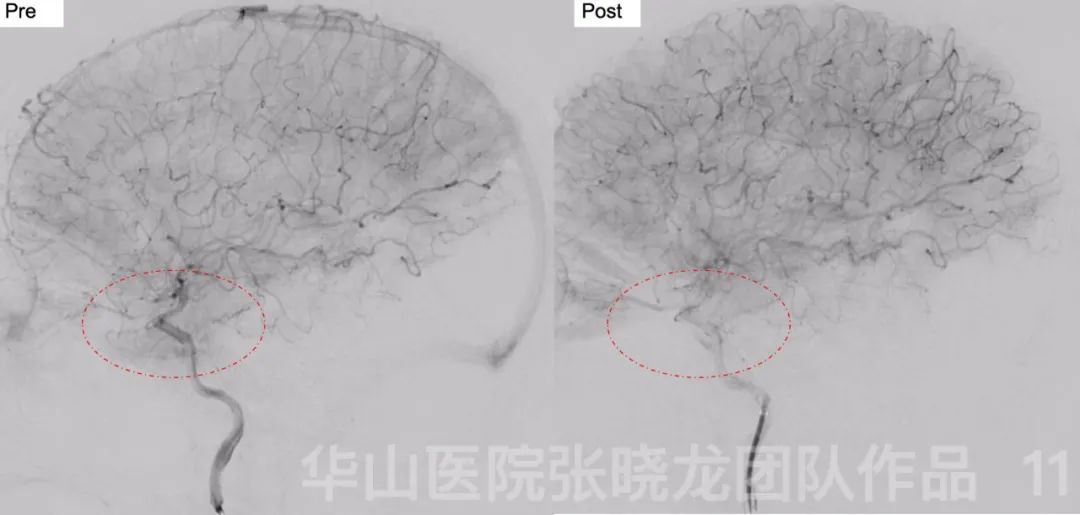
Figure 11. The territory of the occluded MCA branch decreased after operation.
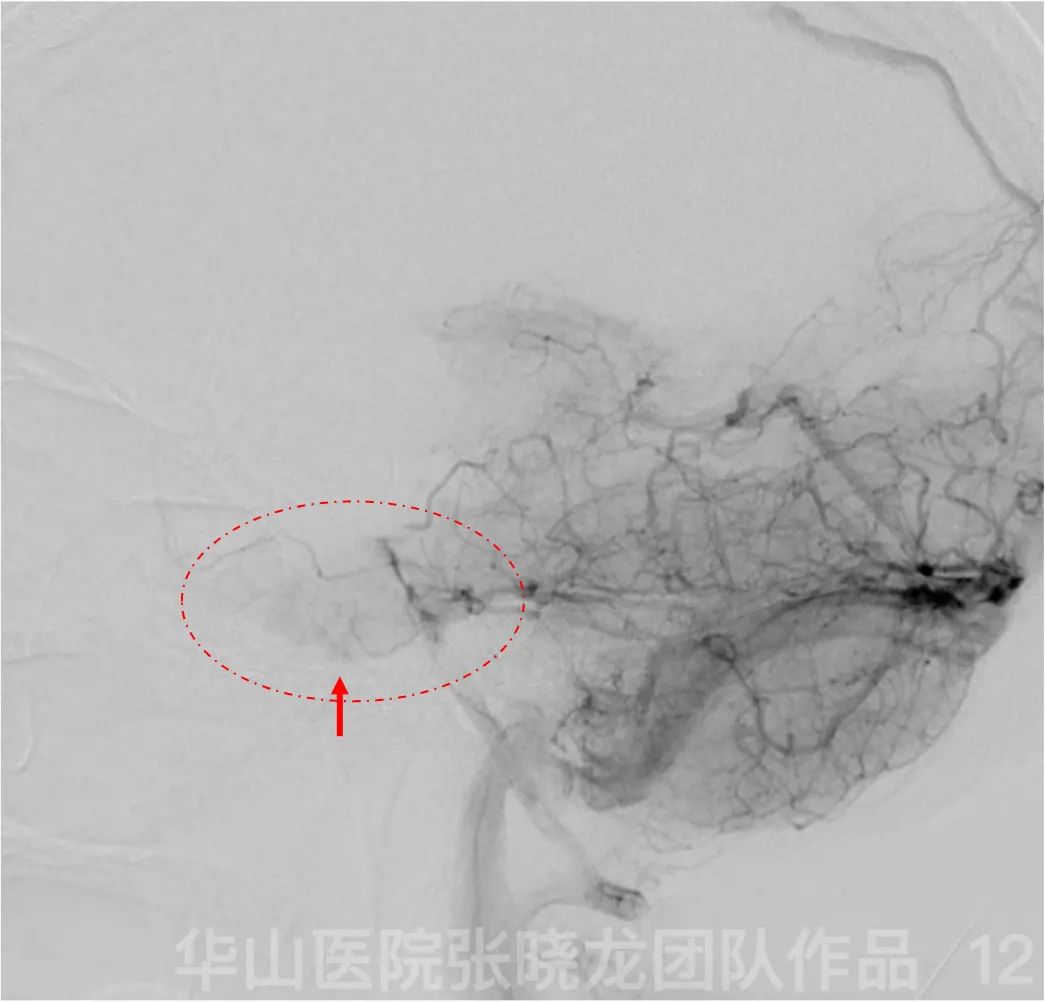
Figure 12. Posterior circulation compensates the region of the occluded MCA branch.
Figure 13 GIF. Dyna CT showed no hemorrhage. Nimodipine 1ml and Tirofiban 6ml were given via the guiding catheter.
3
Post-operation
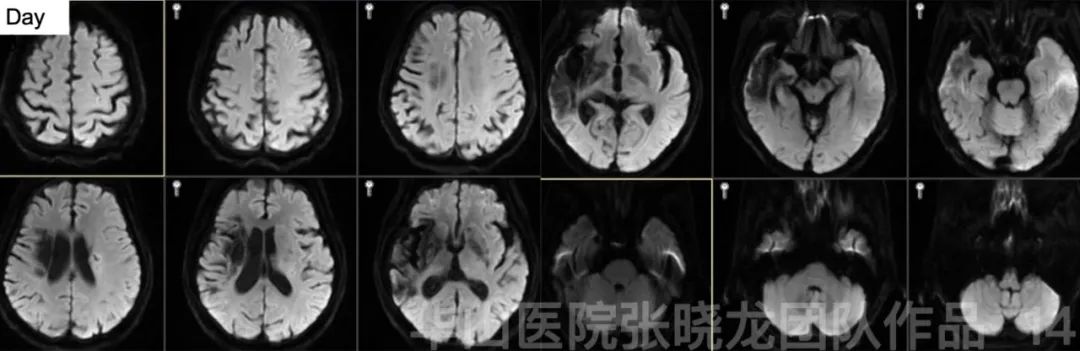
Figure 14. Three-day post-operative MRI DWI shows no acute infarction.
4
Summary
• CTP is unnecessary for the large area chronic infarction; while endovascular therapy spansents a high risk of hemorrhage. After balloon angioplasty was performed, CTA revealed re-stenosis. Furthermore, the symptoms continued and worsened, therefore stenting is necessary.
